Publications
Evaluating Dendritic Cell Reprogramming in Patient-derived Tumor Cells
Abstract
Despite tremendous efforts and achieved advances, cancer is still the leading cause of death worldwide, which underlines the need to develop novel curative approaches. In the past decade, we witnessed the rapid development of immunotherapy – novel treatment strategies based on harnessing the patient´s very own immune system to fight cancer. Although immunotherapy revolutionized the treatment in multiple malignancies, including advanced melanoma, in the vast majority of patients the response is very limited.
Recently, the Pereira lab at Lund University identified a combination of three proteins, PU.1, IRF8, and BATF3 (PIB) which were sufficient to generate immunogenic type 1 dendritic cells from mouse fibroblasts via direct cellular reprogramming. These new cells had a transcriptional program and cell morphology resembling conventional DC type 1 (DC1), which are specialized in antigen cross-presentation and initiating cytotoxic T cell responses. Furthermore, preliminary data has shown that the reprogramming towards dendritic cell fate can also be applied in cancer cells directly. Therefore, inducing antigen presentation directly in tumor cells may help to bypass current limitations of other immunotherapies, such as tumor cell heterogenicity, immune evasion, and neoantigen identification.
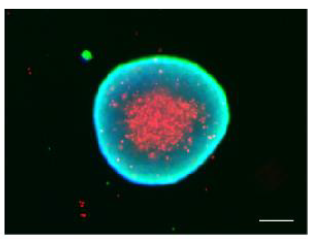
Now, to support the translational efforts of these findings, the application of dendritic cell reprogramming was tested in patient samples. I investigated the reprogramming efficiency mediated by PIB in cancer samples across several malignancies including breast, lung, bladder, pancreatic, head, and neck carcinomas and melanoma as well as cancer associated fibroblasts. I have further evaluated the global gene expression reprogramming at the single cell level with a focus on DC1- and antigen presentation-specific genes. Overall, I observed that all patient samples underwent significant changes during reprogramming with more than 50% of the cells expressing at least one of the reprogramming markers CD45 or HLA-DR. Particularly, lung carcinoma showed highest reprogramming efficiency where more than 60% of the cells were partially reprogrammed and 15% were fully reprogrammed. Interestingly the reprogramming efficiencies observed from patient samples were higher than cancer cell lines, showing a convergent global switch in the transcriptional program to the DC1 fate at the single cell level. Moreover, I also evaluated the reprogramming efficiency in cancer cells tumor organoids constructed by the forced-floating method. Tumor organoids were reprogrammed in similar patterns as their parent cells cultured through conventional 2D methods. However, in the 3D models, it was observed low transduction efficiency, hinting at the potential need to improve the delivery system of PIB into tissues.
These findings support the application of DC reprogramming in patients across multiple malignancies, thus paving the way for the development of a novel cancer gene therapy approach based on dendritic cell reprogramming.