Publications
Generating Dendritic Cells by Direct Cell Reprogramming
June 10, 2021
PhD. Thesis - Lund University
Fábio Alexandre Fiúza Rosa
Resources:
Abstract
Cell fate reprogramming towards pluripotency or alternative somatic cell-types has highlighted the plasticity of adult somatic cells, providing new technologies to generate desired cell types for tissue repair or for disease modeling. There is momentum to bring these concepts to immunology by specifying unique immune cellular identities that set in motion immune responses. Dendritic cells (DCs) are professional antigen presenting cells specialized in the recognition, processing and presentation of antigens to T cells, inducing adaptive immune responses. Within the DC compartment, conventional type 1 DCs (cDC1s) excel in antigen cross- presentation, a critical step to initiate cytotoxic T cell responses. Recent studies have highlighted complementary local and systemic roles of cDC1s in inducing anti-tumor immunity. Nevertheless, their rarity in peripheral blood and the lack of methodologies enabling the generation of a pure population of mature cDC1-like cells limits their study and therapeutic utility. Here, I explore direct cellular
reprogramming from non-hematopoietic cell-types as an alternative approach to generate cDC1.
In this thesis, I screened 34 transcription factors and identified PU.1, IRF8, and BATF3 as the minimal combination required to reprogram mouse and human fibroblasts into cDC1-like cells. Induced DCs (iDCs) generated by cell
reprogramming acquire a DC-like morphology and express cDC1 surface markers and surface molecules required for antigen presentation to T cells. I used single- cell mRNA sequencing to explore the gradual and asynchronous nature of DC reprogramming and demonstrated the downregulation of fibroblast and cell cycle progression genes coupled with the upregulation of cDC1 and antigen presentation genes. Importantly, this approach generated exclusively cDC1-like cells, and not DCs from other subsets. Reconstruction of successful human DC reprogramming trajectories highlighted gene modules associated with successful reprogramming and identified inflammatory cytokine signalling and the DC-inducing transcription factor network as key drivers of the process. Motivated by these observations, I
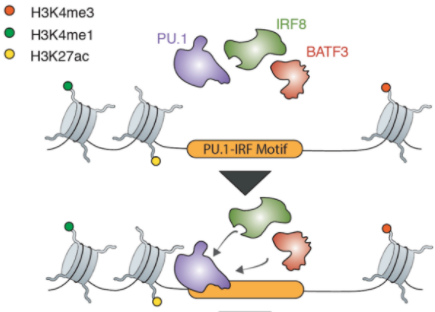
combined IFN-γ, IFN-β and TNF-α with constitutive expression of PU.1, IRF8 and BATF3 to increase human DC reprogramming efficiency by 190-fold. Functionally, iDCs respond to inflammatory stimuli, engulf dead cell material, secrete inflammatory cytokines and cross-present antigens to CD8+ T cells. Interestingly, I observed that intra-tumoral vaccination in syngeneic mouse models increased infiltration of antigen-specific CD8+ T cells, promoted a T cell cytotoxic profile in draining lymph nodes and controlled tumor growth. Mechanistically, I
show that PU.1 displays dominant and independent targeting capacity by engaging enhancer and promoter regions in open chromatin and recruiting IRF8 and BATF3 to the same binding sites. This cooperative binding allows the downregulation of fibroblast genes and activation of cDC1 genes required to achieve DC reprogramming. Finally, I adapted the DC reprogramming protocol to allow high- content screening of small molecules and identified several small molecules that increase reprogramming efficiency and potentially replace the action of PU.1, IRF8 and BATF3 in DC reprogramming.
These findings should open avenues to better understand cDC1 specification and
functional specialization. Ultimately, DC reprogramming might represent a platform for the future generation of cDC1s for therapy.